Home > Advocacy & Policy > Policies Affecting GI > Patient access to colorectal cancer screening
Patient access to colorectal cancer screening
Despite recent victories, patient cost-sharing for CRC screening remains common practice. This financial barrier prevents many Americans from receiving a potentially live-saving screening.
AGA position: Reduce barriers to screening and require all payors public and private to cover the full screening continuum
CRC screening cost-sharing is unacceptable
Passage of the Affordable Care Act (ACA) marked a major victory in the fight against cancer. The law waives coinsurance and deductible for many colorectal cancer (CRC) screening tests, including colonoscopy, sigmoidoscopy and fecal immunochemical test (FIT).1 For many years, Medicare beneficiaries were subject to financial surprise bills when their screening colonoscopy required polyp removal and the screening was classified as therapeutic. In 2020, Congress finally closed this financial loophole by phasing out the coinsurance between 2022 and 2030.
In January 2022, the Biden Administration issued guidance to private health insurance plans clarifying patient cost-sharing for preventive benefits under the ACA, including the new United States Preventive Services Task Force (USPFTF) screening guidelines that recommended colorectal cancer screening begin at age 45.2
The Departments of Labor, Health and Human Services and Treasury, which share jurisdiction over regulating private health insurance benefits under the ACA, stated:
Plans “must cover and may not impose cost sharing with respect to a colonoscopy conducted after a positive non-invasive stool-based screening test or direct visualization screening test for colorectal cancer for individuals described in the USPFTF recommendation.” The agencies state that the “follow-up colonoscopy is an integral part of the preventive screening without which the screening would not be complete.”
Plans are required to implement the new USPFTF screening benefit for those 45 and older for plan or policy years beginning on or after May 31, 2022.3 For health insurance plans that have already been implemented, please check with the insurance provider as they may not include this benefit until next year.
While AGA is pleased with this clarification and believes it will help provide patients with greater screening options and coverage of a complete screening, AGA believes that this policy should also be applied to the Medicare program and urges the Centers for Medicare and Medicaid Services to use its authority to define the screening continuum and correct this lapse in CRC screening coverage for Medicare beneficiaries.
Cost sharing creates financial barriers, which discourages the use of recommended preventive services. Despite recent changes that have eliminated copays and deductibles for patients, there is evidence that consumer cost sharing remains common. In fact, recent studies found that cost sharing for CRC screening occurred in 48.2% of patients with commercial insurance and 77.9% of patients with Medicare coverage.4 Cost sharing also contributes to racial, ethnic and socioeconomic inequities in CRC outcomes.
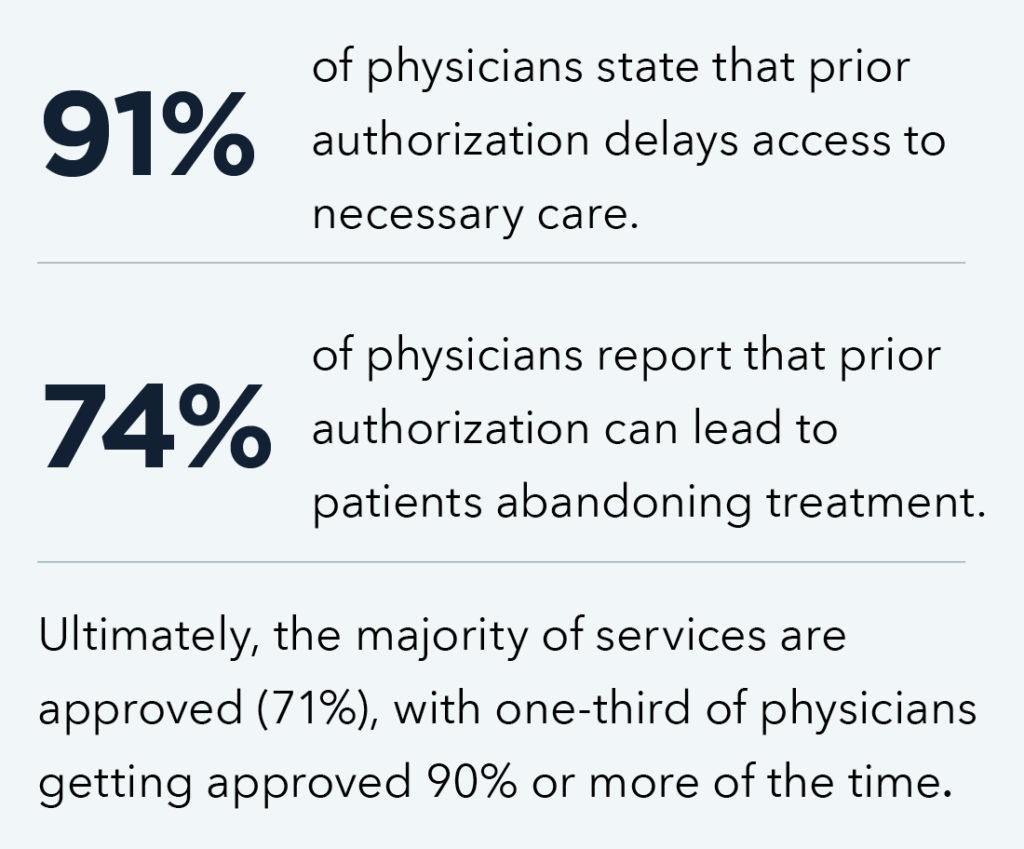
Prior authorization delays care.
This bipartisan legislation aims to increase transparency and accountability of Medicare Advantage plans and streamline the prior authorization process by:
- Establishing an electronic prior authorization process.
- Minimizing the use of prior authorization for services that are routinely approved.
- Ensuring prior authorization requests are reviewed by qualified medical personnel.
- Requiring plans to report on the extent of their use of prior authorization and the rate of delays and denials.
Bottom line: AGA firmly believes that financial barriers must be eliminated and coverage of a complete screening regardless of modality must be consistent among all public and private payors.
1. Sec. 4104 of the “Patient Protection and Affordable Care Act” (ACA) waives the beneficiary coinsurance and deductible for covered preventive services that have a grade of “A” or “B” from the U.S. Preventive Services Task Force (USPFTF). Colonoscopy, sigmoidoscopy and fecal occult blood testing (FOBT) have all been assigned an “A” rating from the USPFTF for adults beginning at age 50 and continuing until age 75.
3. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/colorectal-cancer-screening
4. Fendrick, Mark, Pricnic, Nicole, Miller-Wilson, Lesley-Ann, Wilson, Kathleen, Limburg, Paul. (2021). Out-of-Pocket Costs for Colonoscopy After Non-Invasive Colorectal Cancer Screening Among US Adults with Commercial and Medicare Insurance. Journal of American Medical Association Network Open. 4(12):e2136798. doi:10.1001/jamanetworkopen.2021.36798











