Fellows & Early Career
Fellows & Early Career
Fellows & Early Career Resources
Find articles, education, podcasts, leadership opportunities and more to help you thrive in fellowship and beyond.
Plan your DDW experience
More events
NOV.
30
Six events in 2024
Women in GI Regional Workshops
Network and learn from female leaders in GI dedicated to helping you take the next step in your career.
MARCH
16-17
Academic Skills Workshop
This mentorship-based program is designed to help early career members and fellows successfully start their academic medicine careers. Applications now closed.
Top resources
Continue your education
-
AGA University
Discover upcoming events, webinars and other education to stay current with advances in the GI field.
-
Gastro Cards app
Perfect for clinicians and fellows-in-training on-the-go, Gastro Cards provides instant answers to vexing challenges from endoscopies to IBD.
-
DDSEP Plus
Whether you're preparing for an ABIM exam or just refreshing your knowledge, this comprehensive online platform will help.
Ways to get involved
News directly to your inbox
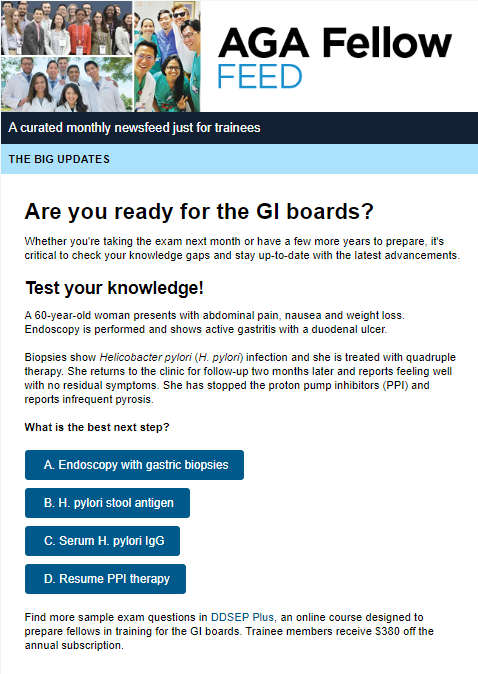
The AGA Fellow Feed is a monthly e-newsletter covering career development, clinical guidance updates and other topics. AGA trainee members receive this resource automatically.
Interested in becoming a member? Learn more here.
Navigating fellowship and beyond
AGA trainees meet up at DDW 2023

























